Understanding how healthcare providers write down their patient details is important for communication in the medical field. SOAP notes offer a simple way for professionals to record information about a patient’s condition, including the subjective and objective sections. Using a SOAP note template helps healthcare workers quickly jot down important details, making sure nothing ever gets missed.
A SOAP note example shows us how this format helps improve communication, reduce errors, and improve clinical hypotheses and clinical reasoning to ensure the right treatment for each patient. This could be used to track subjective objective assessment information or plan next steps.
By using SOAP notes, medical professionals can make their medical records more accurate and provide better care. Let’s explore how this format can improve your patient interactions and care, and give you some free SOAP note templates.
What Does SOAP Stand For?
The SOAP format stands for Subjective, Objective, Assessment, and Plan. It’s a way for healthcare providers to write down what’s going on with a patient in a simple and organized way. This method helps make sure all the important details are there, so everyone involved in the patient’s care is on the same page.
Let’s take a closer look at each part of a SOAP note:
Subjective
The Subjective section is all about what the patient has to say. It’s where they describe how they’re feeling and why they’re there. This includes the chief complaint, or the main reason for the visit, and how the symptoms started, how bad they are, and what makes them better or worse. For example, a patient might say their chest pain hurts more when they exercise.
This section also includes things like the patient’s medical history, what medications they’re on, any allergies, and lifestyle factors like smoking or their job. This helps the provider understand how the patient’s life is being affected by their health problems.
Objective
The Objective section is where the healthcare provider writes down what they observe. This is the measurable stuff, like vital signs (blood pressure, heart rate, temperature), and other measurable data. the client's chief complaint, and anything they find during a physical exam, such as swelling or redness.
This section also includes test results, like blood tests, X-rays, or MRIs. It gives the healthcare provider the clear facts about the patient’s physical condition.
Assessment
The Assessment section is where the healthcare provider looks at all the information and puts it together. They’ll think about the subjective details (what the patient said) and the information (what they observed) to figure out what might be going on. They’ll give their thoughts on what’s causing the problem, including difficulties concentrating, and sometimes, offer a list of other possible causes (called a differential diagnosis).
This is a time for some critical thinking and clinical documentation, figuring out the most likely diagnosis.
Plan
The Plan section is where the provider decides what to do next. This could include things like prescribing medications, referring the patient to a specialist, or recommending changes to their lifestyle to ensure ongoing care . The plan might also include implementation details and instructions for the patient, like what foods to avoid or how much rest to get.
This section usually includes details about when the patient should come back for a follow-up visit, so the provider can see how things are going and make any adjustments to the treatment plan.
11 SOAP Note Template
Here are 11 SOAP note examples from different professions, which can be part of a problem oriented medical record and a helpful free SOAP note template you can use for each:
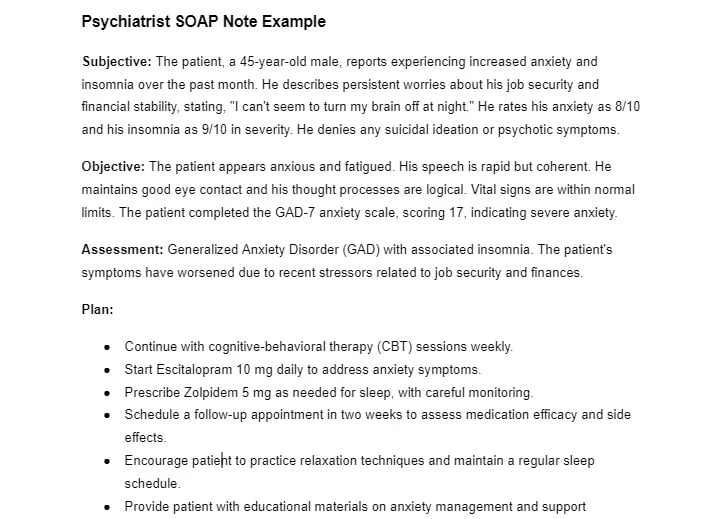
Psychiatrist
A psychiatrist's SOAP note would basically track the patient’s mental health status, including their mood and behavior. Subjective information would come from the patient's own words about their symptoms, while objective data might include findings from psychiatric evaluations. The assessment section would cover diagnoses or changes in mental health conditions, like generalized anxiety disorder. The plan would outline treatment options, like adjusting medications or recommending therapy sessions.
Example:
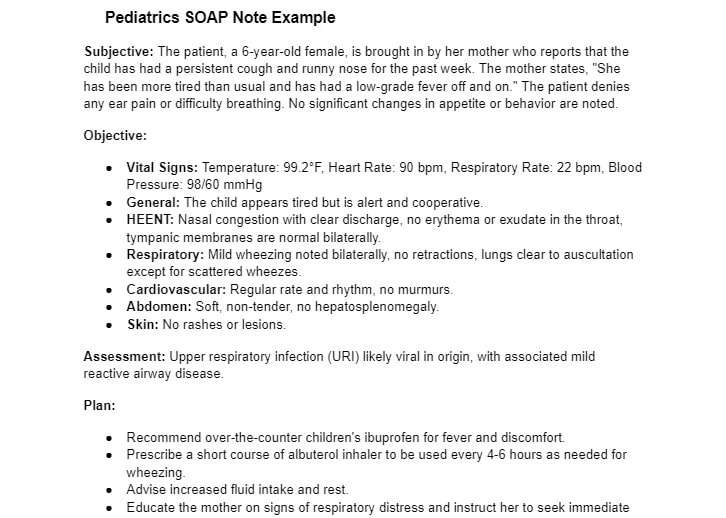
Pediatrics
In a pediatric SOAP note, you'd note the child’s developmental milestones, immunization status, and growth. Subjective information comes from the parent or guardian's report on the child’s health, while objective details include physical exam findings and growth chart measurements. The assessment would highlight any diagnoses, and the plan would set out follow-up visits or referrals.
Example:
Obstetrics
An obstetrics SOAP note documents the expectant mother’s prenatal care. The subjective part might include symptoms such as nausea or fatigue, and could also note any relevant surgical history. In contrast, objective data would involve things like vital signs, fetal heart rate, and ultrasound results. The assessment would evaluate the pregnancy's progress and any complications, while the plan would outline the next steps in prenatal care.
Example:

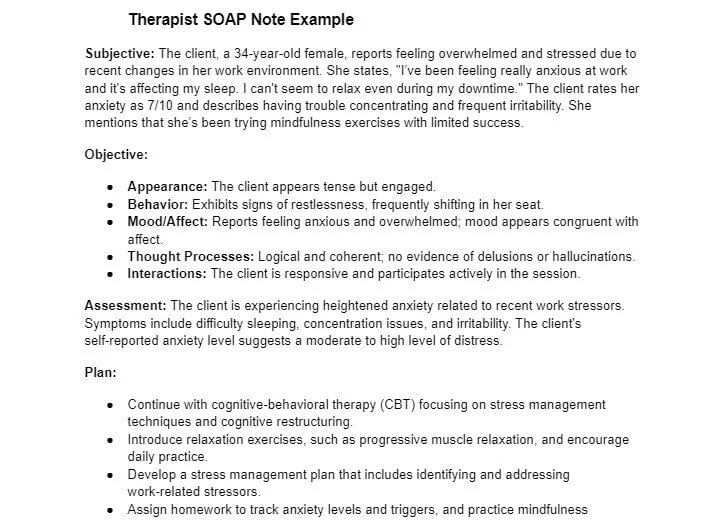
Therapist
For a therapy SOAP note, the subjective section takes note of the client’s feelings and self-reported experiences. Objective information might be the therapist’s observations of the client’s behavior or emotional state. The assessment would evaluate progress toward therapy goals, while the plan would lay out next steps for therapy, including homework or strategies for the next session. This is especially helpful for mental health professionals.
Example:
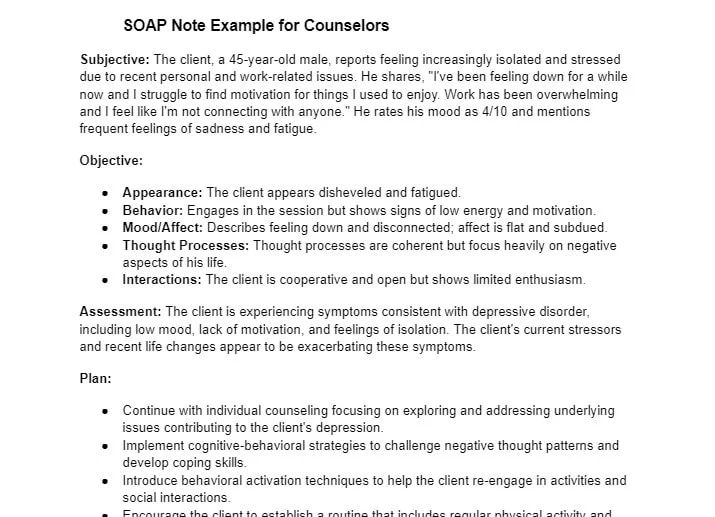
Counselors
A counselor's SOAP note format includes the client’s subjective reports of their emotional and psychological state. Objective observations might focus on the client’s behavior or level of engagement during the session, or group therapy sessions. The assessment provides a clinical impression or diagnosis, while the plan outlines counseling goals and any interventions for future sessions.
Example:
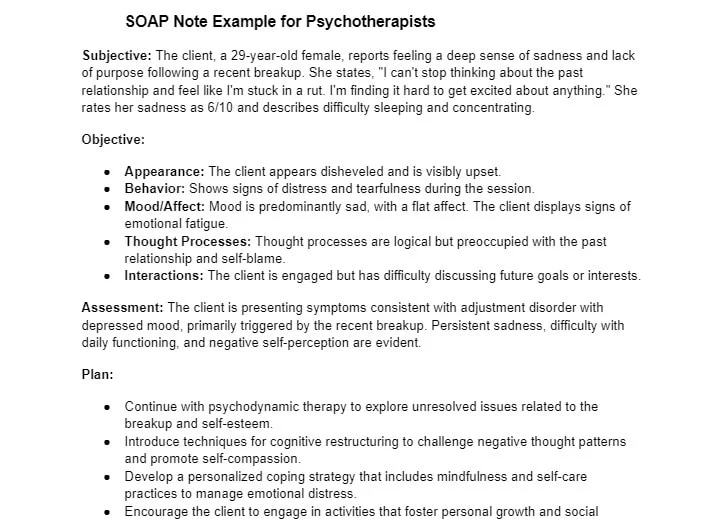
Soap Note Example for Psychotherapists
A psychotherapist's SOAP note tracks the client’s therapeutic progress. Subjective information contains the client’s account of their emotions and life events, including their family history. as well as details about their current medications . Objective data might include observations or psychological test results. The assessment combines these to diagnose conditions such as major depressive disorder and evaluate their progress, while the plan sets goals and therapeutic approaches for future sessions.
Example:
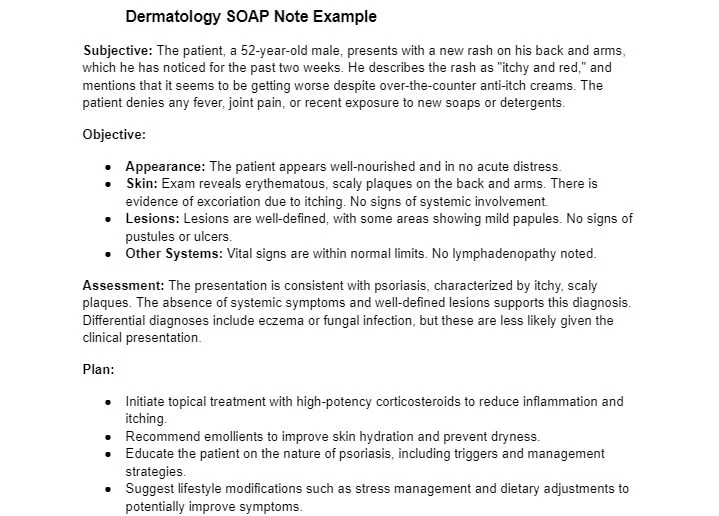
Dermatology
In dermatology, SOAP notes document skin conditions and treatments. Subjective information can also include reports of itching or pain, while objective data tells you the physical exam findings, such as rashes or biopsy results. The assessment will focus on the diagnosis, and the plan might include treatments like medications or lifestyle changes.
Example:
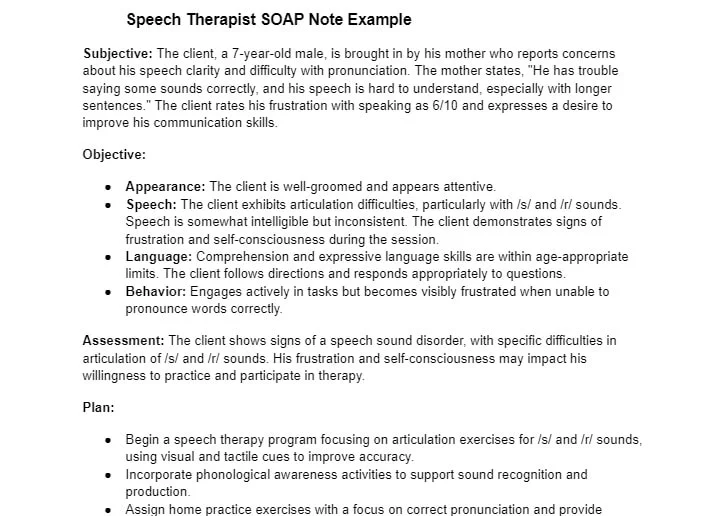
Speech therapist
A speech therapist's SOAP note tracks communication issues and progress. Subjective entries document the client reports or caregiver’s reports on speech challenges, while objective data comes from speech assessments and therapy observations. The assessment evaluates the client’s progress based on the medical notes, and the plan details therapy activities, homework, and goals for upcoming sessions.
Example:
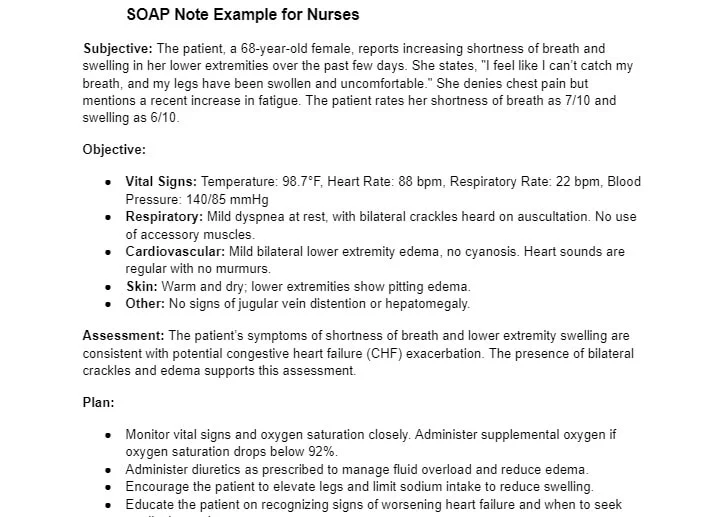
Nurses
A nurse's SOAP note covers a wide range of patient care details. Subjective information may include the patient’s description of symptoms, while objective data covers vital signs, physical findings, and lab results. The assessment provides an overview of the patient’s condition, and the plan includes nursing interventions, patient education, and follow-up plans.
Example:
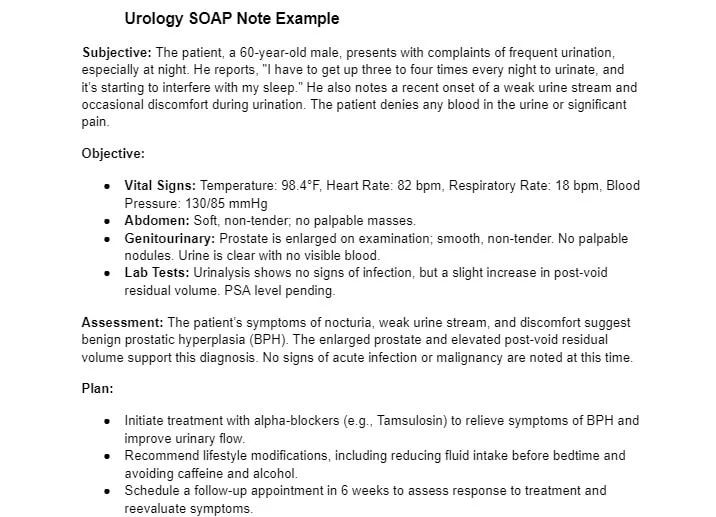
Urology
In urology, the SOAP format focus on patients’ genitourinary issues. Subjective information includes the patient’s report on symptoms like urinary frequency or pain, while objective findings involve more physical exams, urinalysis, and imaging results. The assessment provides a diagnosis of their present illness, and the plan includes treatments and follow-up care.
Example:
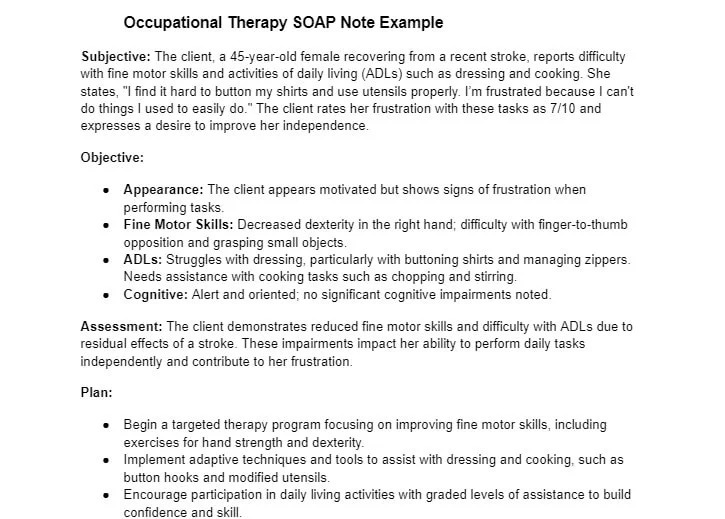
Occupational therapy
Occupational therapy SOAP notes track your patient’s abilities to function. Subjective entries document the patient’s or your caregiver’s reports about daily activities, while objective data includes observations from motor skill assessments. The assessment identifies areas of progress or ongoing challenges, while the plan outlines therapeutic interventions, adaptive equipment suggestions, and future goals.
Example:
Common Mistakes To Avoid When Writing SOAP Notes
1. Leaving Out Important Details
One of the biggest mistakes you can make when writing SOAP notes is forgetting to include key details that could really affect a client’s care, such as the subjective and objective information. It’s not just about the main symptoms - they could also be dealing with other issues, like past medical history, medications, or even things like work stress or family problems. For example, if a client mentions they’ve been stressed because of a recent job loss, that can be just as important as noting their signs.
Making sure you include all the relevant information helps create a complete picture of your client’s health and present illness, which makes it easier to diagnose and plan the right treatment. Don’t skip any details, no matter how small they might seem to you, they all matter in making sure the client gets the best care.
2. Missing the Significance of Findings
Another common issue we found is simply listing observations without taking the time to explain why they matter. For instance, if a client has a fever, it’s not enough to just write that down. You need to think about why that fever is important and what it might mean in the context of their overall health, symptoms, and medical history.
It’s important to give context and explain why certain findings are significant. This helps to clarify your reasoning and ensures that the SOAP note makes sense to anyone else reading it, whether it's for future care or billing.
3. Not Being Specific Enough
Vague or unclear notes can create confusion and lead to mistakes in client care. Instead of just writing something like “Client feels better,” be specific - reflecting on the past week, “Client reports pain has decreased from 8/10 to 4/10 after medication.” Specific details help everyone understand exactly what’s going on and make it easier to track progress.
For symptoms like a cough, don’t just say “Client has a cough.” Describe it - whether it’s dry or productive, how long it lasts, or any other important details. The more specific you are, the clearer the picture becomes, which helps you make more informed decisions in your SOAP notes.
4. Failing to Record the Client's Direct Quotes
Leaving out the client’s own words can mean missing out on valuable insights into how they’re feeling. Direct quotes are important because they give a clearer, more personal view of the client’s condition, for instance, what the client states about their pain, helping you to understand what they’re going through. Sometimes, a client might describe their pain as “a sharp, stabbing pain that feels like a knife,” which gives a much better sense of what they are currently experiencing than simply noting "pain."
Including their own words makes the treatment plan more aligned with their needs, and helps the client feel heard and understood. It also strengthens the therapeutic relationship and ensures you’re working together towards their recovery.
5. How Accurate SOAP Notes Can Help Your Practice
Accurate, detailed SOAP notes don’t just help with your patient care - they can also satisfy requirements for the insurance company and improve your practice’s bottom line while reducing therapist burnout. Clear notes ensure that all services are documented properly, reducing the chances of claims getting denied and ensuring correct billing.
Good SOAP notes also make life easier for therapists, freeing up time that would otherwise be spent on paperwork. This gives you more time to focus on your clients. Plus, thorough documentation helps improve the continuity of care, which leads to better patient outcomes and can even bring in more referrals. When you don’t have to worry as much about administrative work, you can cut down on stress, avoid burnout, and feel more satisfied in your role.
Common Challenges in Writing SOAP Notes
Writing SOAP notes can be a little time-consuming and challenging. Here are some common issues in medical documentation how to manage them:
- Burnout: Take short breaks and delegate tasks when possible. Consider using AI-powered tools to reduce mental fatigue.
- Complex info: Use simple, concise language to communicate complex conditions. Focus on key symptoms and treatments.
- Forgetting details: Use checklists to make sure no important information is left out. Collaborate with your team to stay on top of changes in the patient’s care.
- Inconsistencies: Standardize your approach with templates to keep your notes consistent and clear.
- Time constraints: Set aside time immediately after each patient to write notes, or use voice-to-text tools to speed up your documentation.
Conclusion
Getting the right information during sessions or consultations is quite important for staying on track and reaching your goals. Traditional note-taking can be time-consuming, often causing major details to slip through the cracks and making it harder to fully understand what was being discussed. Using a SOAP note template helps keep things organized and makes decision-making smoother.
But writing SOAP notes by hand can feel like a chore. That’s where Bluedot AI note taker saves the day. Bluedot is a free AI scribe that handles the heavy lifting for you - automatically recording, transcribing your sessions, generating SOAP notes for your meeting templates, and sending follow-up emails tailored to what you need.
Whether it’s for note-taking, meeting templates, follow-ups, or recording meetings, Bluedot makes everything easier. With its transcription available in over 100 languages, it’s especially useful in the medical field.